45.
How Community Health Workers Benefit Ag Communities
44.
Why All Healthcare Providers Need to Understand Agricultural Producers
43.
ATV and UTV Safety in Agriculture
42.
Farm Accidents and Traumatic Injuries - What To Do Before EMS Arrives
41.
Advice on Keeping Your Retired Farm Parents Active and Happy
40.
Why You Should Keep Naloxone on the Farm
39.
Motherhood, Farming, and Invisible Burdens
bonus
Announcement - Brief Hiatus
38.
Manure Management and Safety
37.
One World, One Health
36.
Zoonotic Diseases, Vaccines, and You
bonus
Announcement - Brief Hiatus
35.
All About Ag Youth and Vaping
34.
How Farmers Can Beat the Heat This Summer
33.
Heart Health for Farmers
32.
A Lens to Understand Farmer Stress
31.
Finding Resiliency During Financial Strain
30.
How Ergonomic Technology Can Improve Farm Safety
29.
Farm Safety Tips for Animal Handling
28.
Latino and Hispanic Farmworker Health
27.
Veteran Farmers: Resources and Beekeeping
26.
Farm Stress, Success, and Your Family
25.
HR Management Yields Results
24.
Bonus Episode: Zoonotic Diseases
23.
Rural Telehealth - Part 2 of 2
22.
Rural Telehealth - Part 1 of 2
21.
Youth Stressors and Mental Wellness
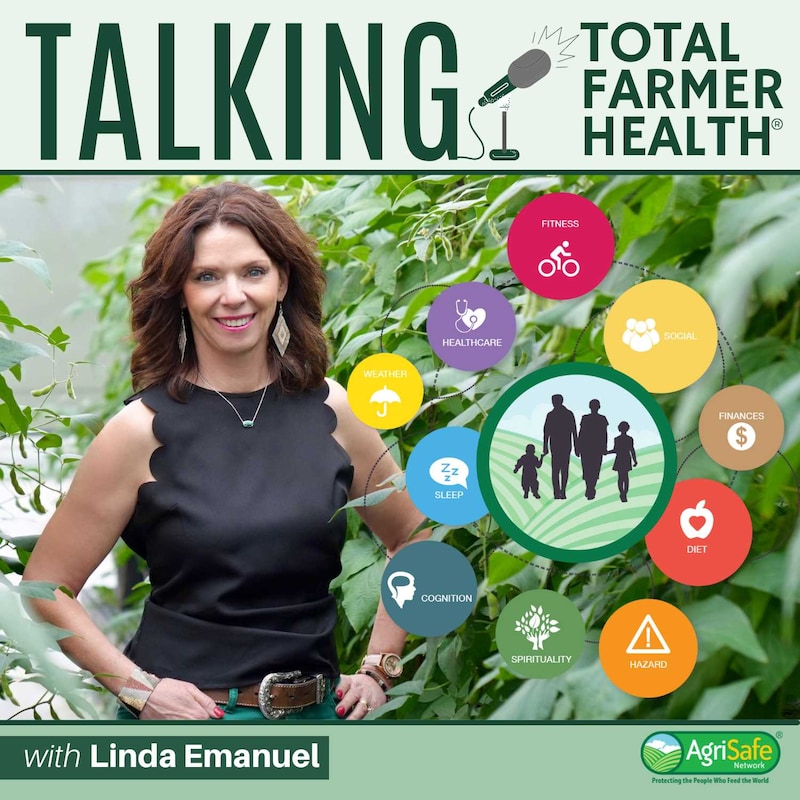
19.
Total Farmer Health Model
17. bonus
Bonus Episode: Women for the Land from American Farmland Trust
16.
Sleep and Your Health
15.
The National AgrAbility Project
14.
Concerns for Older Adults Working in Agriculture
11.
Mental Health Resources for Farmers
9.
Youth Safety on the Farm
2.
Alcohol Use in Agriculture
trailer
Welcome to AgriSafe Talking Total Farmer Health Podcast!